Communicating a prediabetes diagnosis with a patient
Prediabetes: Understand it before you explain it
Prediabetes is one of the most common results GP registrars will encounter in both real consultations and the SCA.
Some candidates may over-alarm:
“You’re nearly diabetic, this a is warning shot!”
Others minimise:
“It’s nothing to worry about you don’t have diabetes yet!”
Prediabetes is best understood (and best explained ) as an early metabolic dysfunction and a window of opportunity.
What Is Prediabetes?
When I was a training as a GP I was once told I should NEVER use the word “sugars” when talking about diabetes and use the word “glucose" instead. I have tried using both words with patients. Often for my patient population the word “sugars” lands well, but you might prefer to use the word “glucose”.
Prediabetes, also called non-diabetic hyperglycaemia, means blood glucose levels are higher than normal but not high enough to diagnose type 2 diabetes.
In UK primary care, this is usually defined using HbA1c:
Normal: < 42 mmol/mol
Prediabetes: 42–47 mmol/mol
Type 2 diabetes: ≥ 48 mmol/mol
This is not a cliff edge - it’s a scale or spectrum
Using a Scale: How I Explain HbA1c to Patients
One technique I often use in consultations is to draw a simple scale. I sketch a horizontal line and label:
Normal on the left
Prediabetes in the middle
Diabetes on the right
This reinforces that movement back left is possible
A typical explanation might be:
“If we think of blood sugar on a scale, this end is normal, this end is diabetes, and you’re here in the middle zone (borderline).”
What’s Actually Going On?
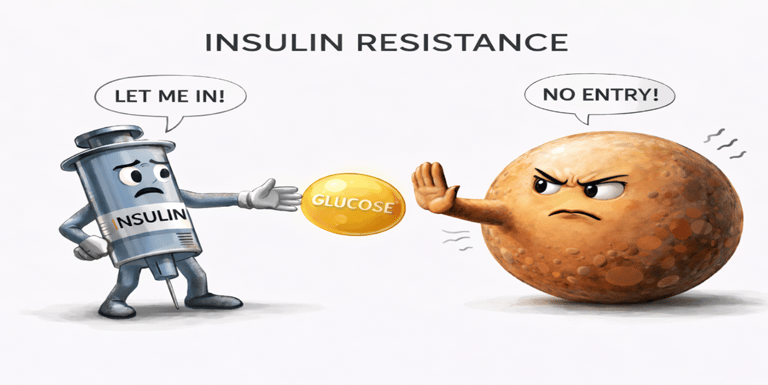
Prediabetes is not primarily a sugar/glucose problem. It is an issue of insulin resistance.
Let look at it step by step
Insulin is released into the blood via the pancreas in response to a rise in blood sugar/glucose levels. Insulin helps move glucose from the blood into cells
Over time, cells can become less responsive to insulin- so less of the blood glucose is being transferred into the cells
The pancreas compensates this rise in blood glucose by producing more insulin
But as the cells are becoming more insulin resistant the amount of insulin being released is never high enough to drive the glucose into the cells.
Blood glucose levels then rise---HbA1c drifts into the prediabetes range
At this stage:
Insulin levels are often high
Pancreatic function is still relatively preserved
This is why prediabetes is often reversible as reducing insulin resistance can improve blood glucose
What Causes Insulin Resistance?
While excess weight can contribute, insulin resistance is multifactorial. Contributors include:
Diets high in ultra-processed foods with high saturated fats and refined carbohydrates
Low fibre intake
Physical inactivity (especially loss of muscle insulin sensitivity)
Poor sleep and chronic stress
Genetic and hormonal factors (e.g. PCOS, gestational diabetes history)
Gut Dysbiosis and Insulin Resistance. Is There a Link?
In simple terms: Yes!
Low-fibre, highly processed diets reduce beneficial gut bacteria
This reduces short-chain fatty acid production SFA (e.g. butyrate) which are anti-inflammatory
Low-grade inflammation increases
Inflammation interferes with cell insulin signalling causing insulin resistance
This helps explain why:
Metabolic health and weight don’t always correlate
HbA1c can improve before significant weight loss occurs
Why Food Quality Matters – its not just about calories
This is why managing prediabetes is not simply about losing weight. Helpful dietary patterns include:
Reducing ultra-processed foods
Increasing prebiotic fibres (vegetables, legumes, whole grains)- to decrease inflammation and decrease insulin resistance (increase the SFA)
Stabilising post-meal glucose responses
SCA Explanation
In your exam you don’t need to go into as much detail as above but its important you emphasise that its multifactorial and there many things a patient can do to help reduce their insulin resistance and blood sugar/glucose levels.
Try saying something like below, but use words and phrases that are comfortable to you. I have put a lot of talking in here and you don’t need to say all of this. Though, you might find some of the phrases below useful.
Option 1 (talk about insulin)
“Your blood test shows something called prediabetes. Have you heard of this before?”
"I often like to explain this using a blood sugars scale. At one end is the non-diabetic range, at the other is diabetes, and you’re here in the middle- its means you have a borderline result"
“The body’s blood sugar level is reduced by a hormone called insulin."
A reason why a persons blood sugar level can move in the prediabetic range is due to issues with insulin resistance"
"When the body is starting to resist insulin ( and we can talk why this may happen) the blood sugar levels rise."
"Diet, movement, sleep, and stress all affect how well insulin works, and when it doesn’t work as efficiently, blood sugar rises."
"Would it be okay if we went through these one by one, so we can work out how best to help you move back towards the non-diabetic end of this line (or towards the left of the scale?)"
Option 2 (no insulin - this is simpler)
"Your blood tests show a borderline blood sugar level. ( draw the sliding scale). Your blood sugar level can be affected by food, stress, sleep and exercise. Can we go through these one by one to see how we can reduce the blood sugar level?"
Food
“Can you talk me through what you’d eat on a typical day?”
(If needed)
“Roughly how much is home-cooked?”
“What are evenings like for food?”
Movement
“What about movement or exercise - what does a usual week look like for you?”
“Thanks, that gives me a really good picture.”
Sleep
“How is your sleep at the moment?”
“Do you generally wake up feeling rested?”
Stress
"And how are things for you stress-wise at work or at home?”
“From what you’ve told me, it sounds like the areas we could focus on first are xxxxxxx to reduce your blood sugar level
How does that sound to you?”
Summary
I often find with patients when they have booked an appointment for blood tests they want to get those results first not re-hash the history they gave the previous doctor who organised the bloods.
Share their results
Explain what can cause those results
Then take a focused history.
Once you have got the information from the patient you can make a shared personalised management plan (not a generic one ).